by Laura Silvoy (Array Advisors)
As presented at the 2016 Winter Simulation Conference
Abstract
Traditionally, architects rely on average utilization benchmarks to determine appropriate department sizes when planning a new facility. While these averages might adequately predict space for the design of an office building or parking lot, they sometimes fall short of accurately determining the amount of space needed for healthcare facilities. A community hospital in a costal Mid-Atlantic state is experiencing significant emergency department (ED) holds due to a lack of inpatient capacity. Analysis of patient arrival and unit assignment data led the team to believe that treating observation patients in inpatient units is causing the capacity problem. A discrete event simulation (DES) model helped determine the appropriate size of an observation unit needed to reduce ED holds and relieve current inpatient pressures.
Current State
The hospital currently experiences a high volume of holds in the ED. They believe that inadequate capacity in the inpatient units is causing these holds. An addition to the facility included 25 observation beds and a 24-inpatient bed Transitional Care Unit (TCU). Today, due to growth in ED visits, the observation beds are being used as additional ED beds, and the TCU has been designated as the observation and inpatient holding area. Each inpatient bed unit, including Cardiac, Medical and Surgical, has 14 step-down beds and 36 acute care beds. These units are experiencing high utilization rates throughout the year, likely because the TCU beds are not available for their intended use as transition beds for inpatients moving from the ED to an acute care unit.
Future State
Hospital administrators believe that reclaiming the 24-bed TCU will alleviate the capacity strain currently felt in the inpatient units. In order to use these beds as originally intended, a dedicated observation unit will be necessary to accommodate the observation population. Traditionally, the average daily census (ADC) of observation patients would be used to generate a unit size. Unfortunately, since this number is an average, the unit will only be large enough about fifty percent of the time. After spending time and money on an expansion, and living through construction, the facility would still feel the stress of inadequate observation capacity for nearly half of the year if they used ADC to determine unit size. In this case, the observation average daily census is 35 patients. The client is interested in determining how many additional observation beds are necessary to adequately accommodate the observation population and whether reclaiming the TCU will alleviate inpatient capacity strain.
Inpatient Unit Simulation Model
While these may seem like high-level questions that could easily be answered using spreadsheet analysis, the movement of patients through these units is surprisingly complex and best analyzed using DES. In this case, the model includes a simple patient flow in which patients arrive to a unit specified in the data, stay for a length of time based on a distribution derived from actual patient data from the electronic medical record and leave the unit.
After designing a simulation that models where patients are sent today and ensuring that it accurately represents the current system, changes were made to the assigned units for observation patients and inpatients treated in an existing TCU bed. In the first scenario, all observation patients are sent to an infinitelysized observation unit to help the modeler determine a feasible range for the proposed bed count. Patients who were treated in the TCU are still sent to that unit, because it is no longer being used to hold observation patients. This first scenario resulted in very low utilization of the TCU by inpatients, which led the project team to assume that observation patients could use a TCU bed if no capacity was available in the observation unit.
Additional scenarios were developed with constrained observation bed capacities that work with an expected nursing ratio of 5:1. If a bed is available in the limited unit, the observation patient seizes that bed. If a bed is not available, the observation patient “checks” a series of units starting with the TCU, to see if there is additional capacity in another suitable location. If there are still no available beds, the patient will simply wait for an observation bed to become available. Similarly, the inpatients treated in the TCU will first “check” the TCU for available beds, then “check” the Medical, Cardiac, and Surgical units for available beds.
The results produced by the model were somewhat unexpected, but upon further analysis, were determined to be accurate. One surprising result was the size of the observation unit. While the infinite-capacity results suggested that 49 observation beds would be necessary to have a bed available 100% of the time, incorporating the TCU as an option for observation patients led to smaller options for the observation unit and higher utilization rate in the TCU, which resulted in better staffing of the system as a whole.
Results and Recommendations
Overall, the health system needs to balance the utilization of their observation unit and additional inpatient beds gained by reclaiming the 24-bed TCU. Figure 1 shows how utilization of these units changes as the number of observation beds changes. Due to the bed selection assumptions defined above, the TCU will become more utilized as the number of observation beds decreases.
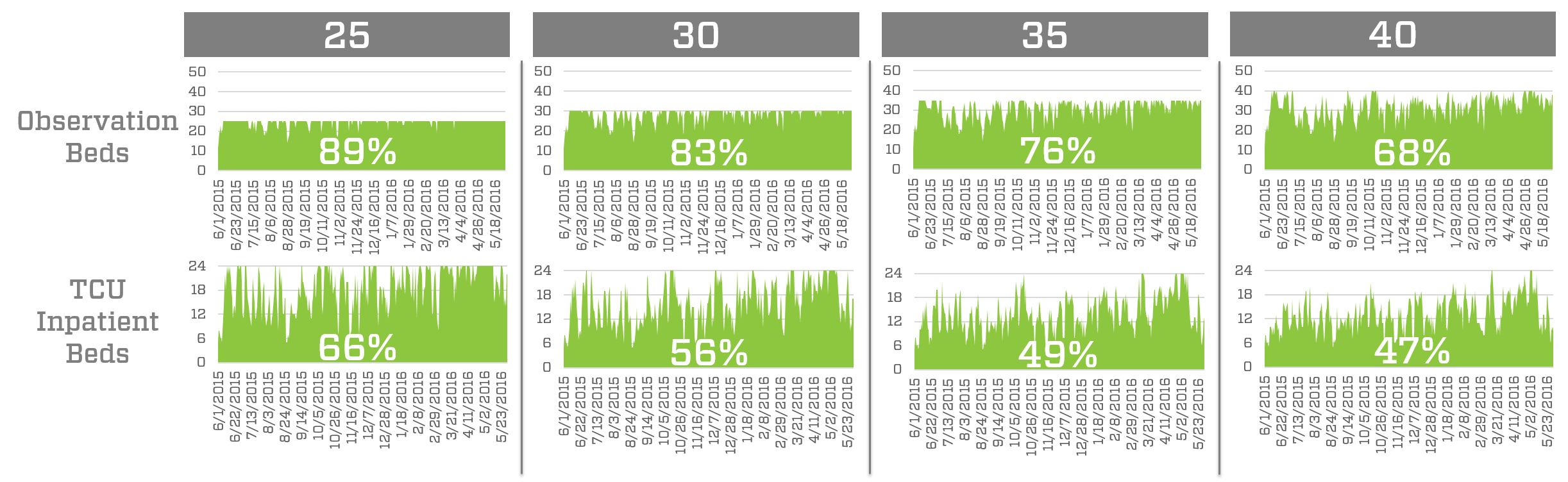
Figure 1: Utilization of observation beds and TCU inpatient beds for four different observation bed capacities.
From the perspective of staffing, it is important to keep a unit utilized about 75% of the time. In an observation unit, where patient length of stay is shorter and more volatile, this utilization might be closer to 70%, but can be higher if the organization is willing to accept a higher risk of a bed not being available when a patient needs it. These constraints led the client to consider the 30- or 35-bed observation units, which generate utilization rates for both the TCU and observation unit that lead to better staffing solutions.
The world of healthcare is complex and questions that arise cannot always be answered with a single solution. Providing this range of options allows the client to see how different observation bed counts impact utilization of the TCU and the observation beds and helps them make a decision quickly and with more confidence than they would have without the results of the simulation model.