Fragmentation is a common problem in the United States healthcare delivery system. For patients with complex medical conditions requiring multiple providers, this problem is particularly perplexing. One solution being developed, called an Integrated Practice Unit (IPU), involves a co-located multidisciplinary team of providers addressing a patient’s medical condition over a full care cycle. In this paper, we use simulation to design a WorkLife IPU that treats medical issues arising in the workplace from minor illnesses to acute non-urgent injuries. More specifically, we determine a patient appointment schedule and the number of resources required to achieve patient throughput, clinic closing time, and patient waiting time targets set by the IPU management.
Introduction
Historically, the United States healthcare delivery system has been fragmented. Thus, patients with medical conditions requiring multiple providers must coordinate and execute their own plan of care. The more complex the condition, the more challenging it is for patients, especially for those from underserved populations. Porter and Teisburg (2006) argue that the root cause for this fragmentation has been competition within the system at the wrong level. More specifically, they contend that competition is either too narrow (e.g., at the level of particular service) or too broad (e.g., at the level of healthcare plans), and should instead “take place for addressing medical conditions over the full cycle of care” (Porter and Teisburg 2006, page 44). The latter has the potential to create greater value for both patients and providers, and to result in more integrated approaches to healthcare delivery
To directly address this issue, Porter and Lee (2013) define the concept of an Integrated Practice Unit (IPU). An IPU is a co-located, multidisciplinary team of providers designed to treat the full care cycle for a specific medical condition. In an IPU, providers move around the patients, rather than patients having to move around to visit multiple providers in different locations. The “specific medical condition” considered in this paper is workplace-related issues ranging from minor illnesses and complaints to acute non-urgent injuries. Other applications being considered include cancer care at the MD Anderson Cancer Center in Houston, TX, a spine clinic at the Virginia Mason Medical Center in Seattle, WA, cardiac and vascular care at Cleveland Clinic in Cleveland, OH (Porter and Lee 2013), and a women’s health clinic and care for a variety of musculoskeletal conditions at the Dell Medical School (DMS) in Austin, TX (Koenig et al. 2016, Morrice et al. 2018)
In this paper, we use simulation to aid in the design of the WorkLife IPU in DMS at The University of Texas at Austin. More specifically, we determine a patient appointment schedule and the number of resources needed to achieve capacity, clinic closing time, and patient waiting time targets. From a scheduling perspective, an IPU may be viewed as an extended combination of a flexible flow shop and an open shop (Pinedo 2016) with multiple patient types on different care pathways through a multidisciplinary team of providers. With stochastic arrival and services times, along with stochastic routing, optimal formulations for determining patient and resource flow are intractable. Another complicating factor is that the IPU faces a mixture of scheduled and walk-in patients. Hence, we resort to simulation.
There are a number of simulation studies on healthcare delivery. Swisher et al. (2001) were one of the first to build a model using an object-oriented simulation package with graphical capabilities. They studied a family practice facility with the goal of maximizing a combination of clinic profit, and patient and staff satisfaction. Results were based on a fractional factorial design that included the number of mid-level practitioners, the number of nurses, the number of medical assistants, the number of check-in rooms, the number of examination rooms, and the number of specialty rooms. In work closely related to ours, White et al. (2011) developed an empirically based discrete-event simulation to examine the interactions between patient appointment policies and capacity allocation policies (i.e., the number of available examination rooms) and how they jointly affect resource utilization, patient waiting time and other performance measures. Data were gathered from an outpatient orthopaedic clinic with two different patient types, five registrars, two radiology technicians, and a single physician. One of the main distinctions our IPU work is the centrality of the patient with providers moving to patients rather than patients moving to different providers
The remainder of the paper is organized in the following manner. Section 2 contains he problem description. In Section 3, we describe the model. Section 4 provides results of our analysis and Section 5 contains concluding remarks.
Problem description
The WorkLife IPU in the Dell Medical School (WorkLife 2018) provides multiple services. It functions as a walk-in clinic treating minor medical conditions (e.g., sprains and strains, colds and flus) and provides common inoculations such as flu shots for workers at nearby businesses. The IPU also serves as an occupational health and injury clinic performing physicals and drug tests, and treating acute non-urgent workplace injuries. To support the occupational side of the business, Worklife provides administrative support to patients and their employers for workers compensation and workplace accidents, as two examples
With numerous services and a coordinated approach to care, the WorkLife IPU is staffed by multiple providers of different levels and sees five different types of patients, each with its own care pathway. The Base Case staff includes a Physician, two Nurse Practitioners (NPs), two medical assistants (MAs), two administrative personnel (referred to as Admins), and one Radiologist. The Physician is resident in the clinic about 40% of the time. Both the Physician and the Radiologist are shared resources with other IPUs in the Dell Medical School. Resources also include four exam rooms and two restrooms for drug screening.
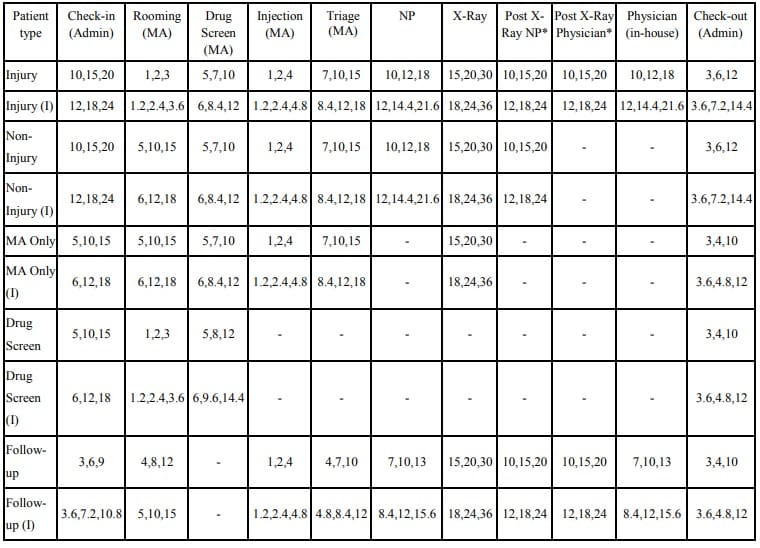
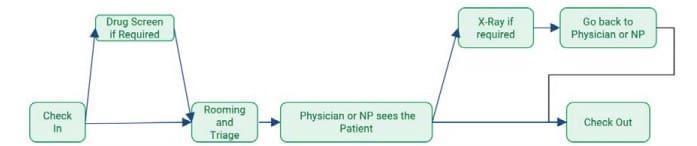
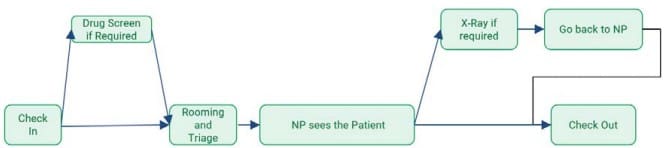
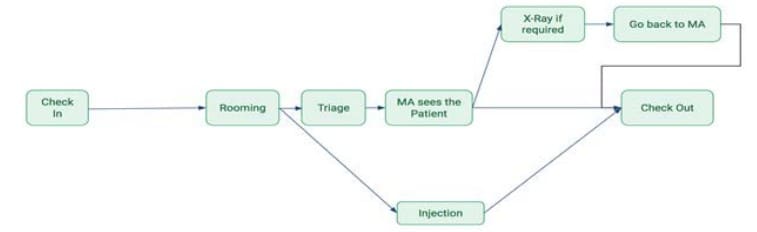
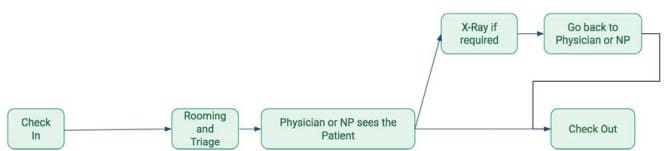
Patients are categorized as Injury, Non-injury, Non-injury requiring MA only (MA Only, for short), Drug Screen only, and Follow-up. The Follow-up patient represents a follow-up appointment from a previous visit for a single incident. Figures 1-5 depict the care pathways for all patient types. Referring to Figure 1, after check-in, Injury patients may require a drug screen. Then they are placed in a room and undergo triage. Depending on the severity of the injury, the patient either sees a Physician or an NP. An Xray is conducted if required, and the patient returns to the provider for treatment. Once treatment is complete, the patient checks out of the clinic. Non-injury patients follow a very similar pathway except they only see the NP (Figure 2). MA Only patients (Figure 3) require minor care and as the name suggests, they only see the MA. Some patients on this pathway only require an injection (e.g., an immunization). The rest follow a pathway that is similar to Injury and Non-injury patients. As Figure 4 illustrates, Drug Screen patients follow a straightforward pathway. The drug screen is conducted by the MA. Follow-up patients follow a similar pathway to Injury and Non-Injury, except none require a drug screen since, if required, this would have been conducted on the initial visit. It is important to note that in an IPU, once a patient is assigned to a room, it remains her room until she goes to check-out. Except for the Radiologist who see patients in a specialized X-ray facility, all providers visit the patient in the room to which she is assigned.

For the WorkLife IPU, about 40% of the patients require an interpreter and those patients spend approximately 20% more time with each provider on average. While the need for an interpreter does not alter the care paths, from a modeling point of view, it does require the need to consider 10 patient types. The follow-up visits constitute about 35% of the patients on any given day. By definition, these are scheduled appointments. The remaining patient types are unscheduled walk-ins.
The WorkLife IPU management asked our research team to help them design a clinic with the following average requirements. First, they wanted to be able to see 55 patients per day. Second, clinic closing time needed to be close to 9 hours (or 5pm in the afternoon since the clinic is scheduled to open at 8am) in order to avoid overtime pay. Third, time waiting for check-in, rooming, and drug screen each needed to be less than five minutes to enhance patient experience. Finally, they wanted to be able to achieve these requirements with a minimal increase in Base Case staffing levels.