by John J. Case, Kimberly P. Ellis
As presented at the 2019 Winter Simulation Conference
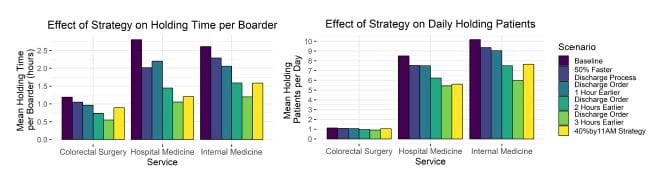
In collaboration with the leadership team at a major metropolitan hospital in the United States, the research team develops alternatives to improve the hospital’s discharge system to increase the availability of bed space for new patients. Following a multi-day site visit, we utilized service time data to develop a discrete event simulation (DES) model to evaluate discharge improvement strategies, assuming fixed capacity. We found that a Percent-by-Time discharge strategy improved the hospital’s patient holding time by a minimum of 24% if implemented in all service areas. This zero-cost strategy requires no increases to hospital resources and can improve patient flow and timely access to healthcare in highly utilized hospitals.
Introduction
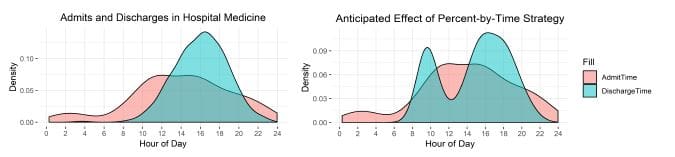
In 2017, a major metropolitan hospital experienced average bed occupation of 93% and periodic unavailability of bed space for new in-takes due to an average intake of 1PM and an average discharge of 3PM. The hospital’s leadership desired to improve the discharge time of day in order to alleviate the scarcity of available bed space for new patient intakes. The authors visited the hospital where we observed patient flow processes, interviewed doctors, nurse practitioners, nurses, social workers, case managers, and housekeeping and administrative staff in multiple surgical and medicinal hospital services.