by Breanna Swan, Osman Ozaltin, Sonja Hilburn, Elizabeth Gignac, George McCammon Jr.
As presented at the 2019 Winter Simulation Conference
Complex interactions between workload variability, uncertain and increasing arrival rates, and resource constraints make it difficult to improve flow through emergency departments (EDs). This complexity causes crowded EDs, long patient lengths of stay, and burnout among care providers. One way to improve efficiency while maintaining high quality care is to switch from a siloed unit-based department to a team-based design or pod system. This paper seeks to compare a pod system against the unit-based design at Southeastern Health’s ED using a discrete event simulation. Robustness of the model under a selection of staffing designs will be tested with increased arrival rates and varying mixes of severity for incoming patients. Ultimately, it is shown the pod system maintains quality of care metrics while increasing resource utilization, establishing proof of concept that an optimized pod system can improve flow in the ED.
Introduction
Emergency Department (ED) crowding due to long patient lengths of stay increases the chances of patient harm and reduces patient satisfaction. Crowded EDs also reduce job satisfaction, reduce productivity, and causes burnout (Wiler et al. 2011). Complex interactions between workload variability, uncertain and increasing arrival rates, and resource constraints make it difficult to improve flow and reduce crowding. The complexity of EDs and the introduction of big data from electronic health records suggest an evidence-based decision tool is vital in supporting ED leadership and policies.
Forecasts of increased healthcare use and decreased resources compound the life-threatening issue of crowded EDs; the American Hospital Association estimates 33% of rural and 69% of urban hospital EDs are functioning at overcapacity yet there continues to be a significant shortfall of registered nurses. Teaching hospitals face additional considerations; residents need quality instruction time from preceptors and hands-on learning experience from patient caseloads which both impact physician efficiency and patient’s length of stay. One proposed method for overcoming these barriers while improving patient care is to redesign siloed ED units into smaller yet more integrated team-based pods which have improved scheduling and staffing flexibility with the ability to balance patient workload amongst teams of care providers.
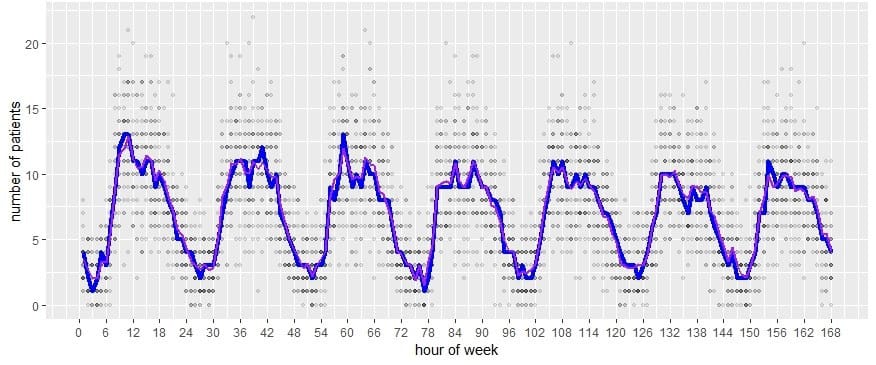
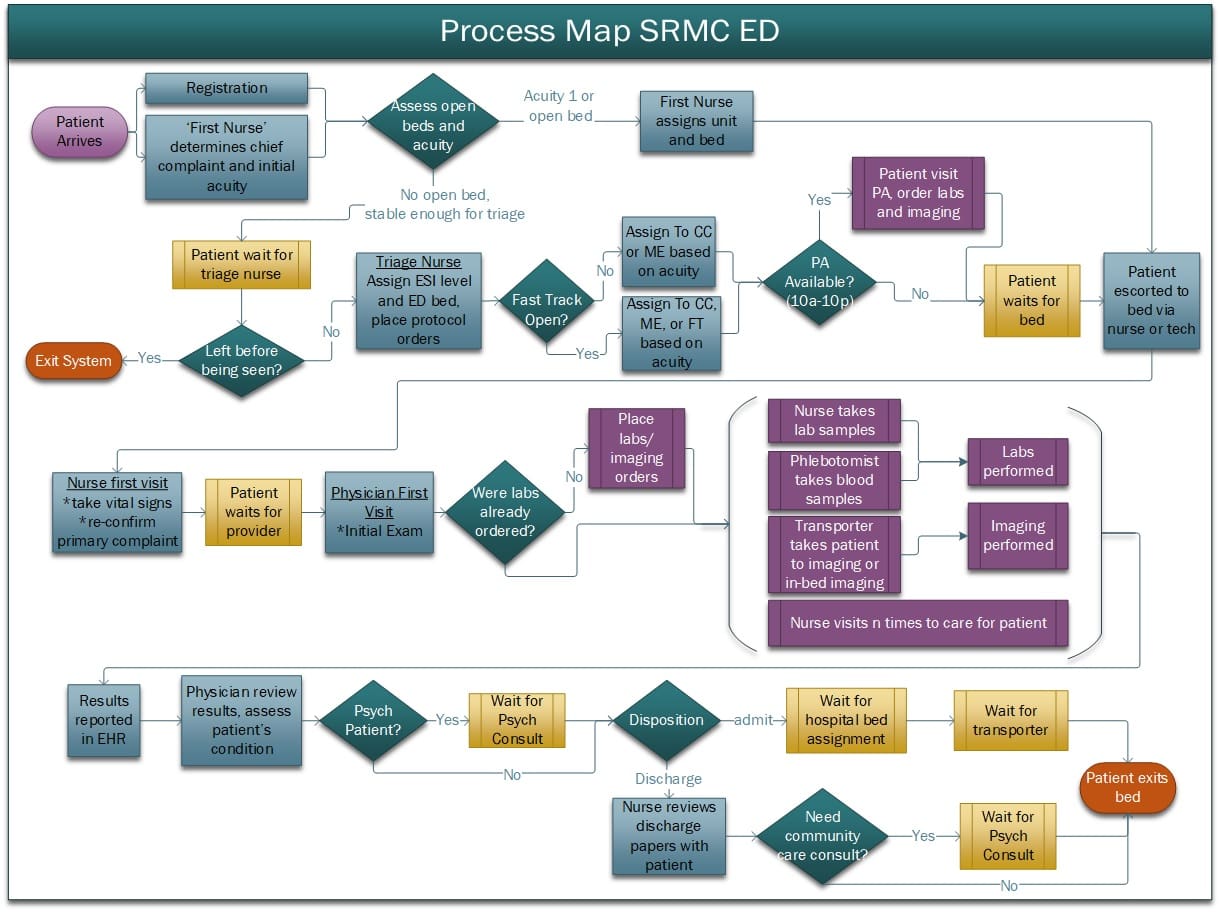
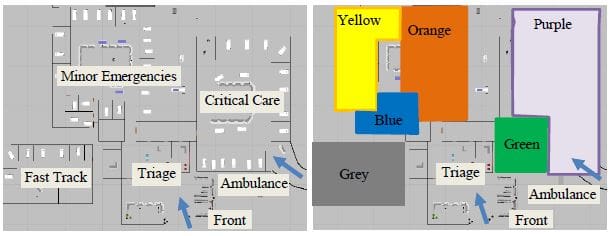
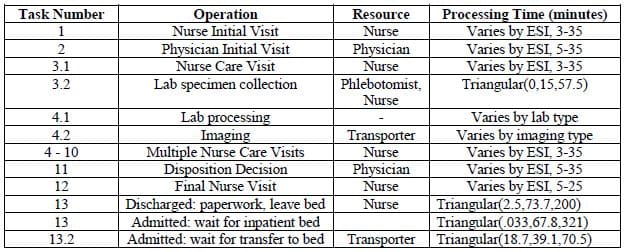
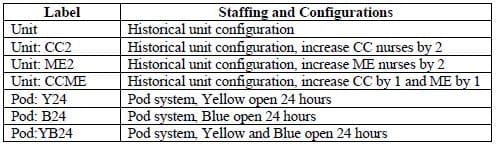
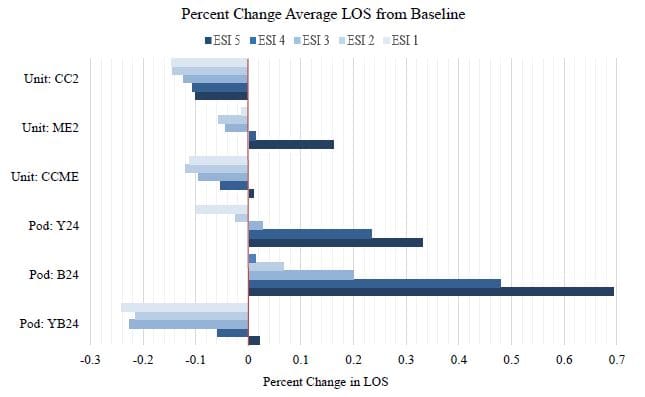
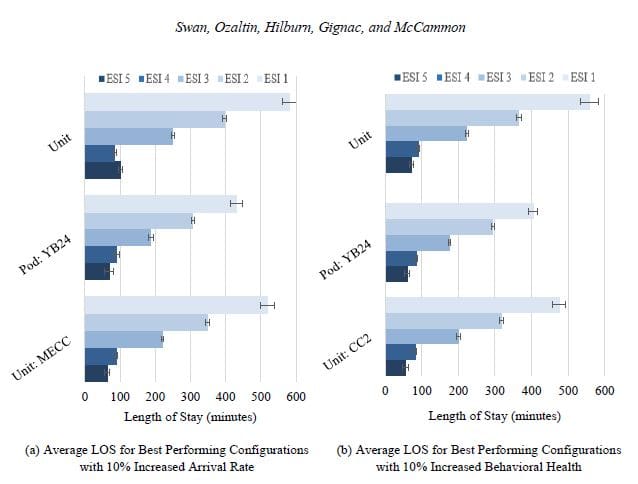
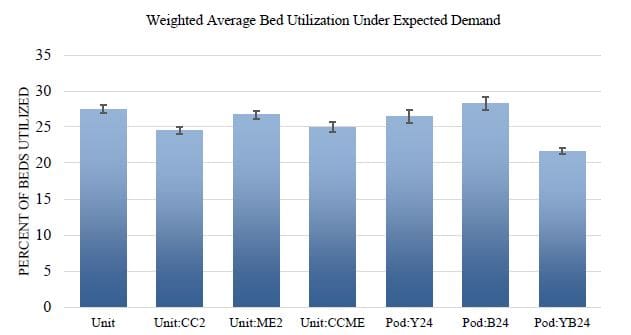
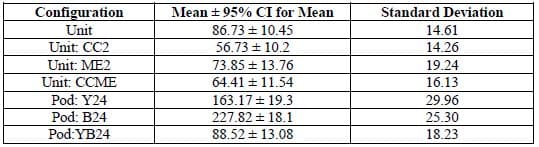
Southeastern Health’s ED, which sees over 170 patients each day, aims to improve patient outcomes and staff experience by reducing patient length of stay by transitioning to a pod system. The purpose of this work is to evaluate and compare performance of a pod design to the current unit design using a discrete event simulation built. Performance and robustness across multiple configurations of staffing models (i.e. number of nurses per shift) and department designs (unit or pod) will be evaluated for expected demand, increased arrival rates, and varying patient severity mix. The key performance metrics are length of stay (LOS) measured by time from registration to discharge, resource utilization, and ED volume (i.e. the number of patients in the ED at a given moment in time).
Relevant Literature
Discrete event simulation (DES) is useful for experimenting with new policies and in preparing for future events such as increased arrival rates or changing staff levels. It has been applied to identify the best patient care pathways, efficiently allocate resources, and determine staffing designs (Oh et al. 2016; Augusto et al. 2018). In particular, Oh et al. used simulation to reduce patient LOS by evaluating and comparing system improvements; they ultimately found reducing adult patient CT scan oral contrast drink time, increased self-dictation use in radiology, and reducing sample re-collection rate had the most influence on reducing LOS.
Transitioning to a pod system requires the redesign of pod scheduling, staff assignments, and patient routing rules. Mixed integer optimization (Sir et al. 2017), simulation models, and queuing theory are techniques used to determine new shift templates for care providers and pod scheduling. Designs vary from physician-led teams assigned to specific beds with each pod randomly assigned patients (Patel and Vinson 2005) to more dedicated pods to suit patient population needs like pediatric and low-acuity specific pods (Oh et al. 2016; Dinh et al. 2015). Routing of patients to pods is critical to flow; Agor et al. developed a workload score to reduce the time the ED spent at maximum utilization. The score considered pod and ED attributes like number of behavioral health patients and queue length (Agor et al. 2016). Finally, new roles such as a navigator overseeing patient flow (Dinh et al. 2015) or a dedicated nurse technician transporting patients to beds may be needed for a successful transition from unit-based designs to a pod system.
Team based care has been studied observationally and in DES models and is shown to reduce time to patient’s first visit with a physician, reduced left without being seen cases, improved patient satisfaction, and reduced LOS while maintaining clinical quality of care (Patel and Vinson 2005; Oh et al. 2016; Dinh et al. 2015). Beyond patient experience, team based care also has been shown to improve staff experience. Teaming residents with a single physician, all seeing common patients, was associated with improved perceptions of quality of teaching (Nable et al. 2014).
The practical successes of a pod-based design in the ED paired with the flexibility of discrete-event simulation modeling suggest that this work can improve ED flow and inform staffing configurations and unit scheduling at Southeastern Health.